According to the Canadian Association of Optometrists, glaucoma is one of the leading causes of blindness in Canada. If left untreated, this serious condition can cause significant permanent visual impairment. That is why patients over the age of 40 typically are screened with cutting-edge OCT. If we suspect that you have glaucoma, we can begin treatment using glaucoma lowering medication eye drops and follow up accordingly.
Glaucoma hits close to home for Dr. Hazan, whose own mother suffers from glaucoma and vision loss. This personal experience has only strengthened his drive to ensure that all patients receive an accurate and timely diagnosis, safeguarding their sight.

What is Glaucoma?
Glaucoma is a progressive disease of the optic nerve (which is responsible for transmitting information from the eye to the brain). The resulting deterioration affects the amount and the quality of information transmitted.
If glaucoma is not detected and treated early, it can lead to irreversible vision loss and even blindness. The peripheral vision is typically affected first, followed by the central vision in the later stages of the disease.
Types of Glaucoma
Four of the more common forms of glaucoma:
Primary open-angle glaucoma is the most common form of glaucoma. Our eyes produce a liquid, called aqueous fluid, which fills the anterior chamber of the eye. When too much of this fluid accumulates, or the fluid within the eye cannot properly drain, it can increase the internal pressure of the eye and damage the optic nerve.
Normal-tension glaucoma occurs when the optic nerve becomes damaged even when the eye’s internal pressure is within normal range. It is possible that individuals who develop normal-tension glaucoma may have incredibly sensitive optic nerves, or their optic nerves are not getting enough blood. This constricted blood supply may be caused by atherosclerosis, which is a hardening of the arteries. In these cases, even normal intraocular pressure may be too much for the optic nerve to bear, resulting in damage.
Secondary glaucoma typically occurs as a result of an injury or inflammation (uveitis) in the eye. This disruption causes the eye’s internal pressure to rise. Some medical conditions, medications, and structural abnormalities within the eye can also cause secondary glaucoma, including, in rare cases, eye surgery.
Angle-closure glaucoma, also called narrow-angle glaucoma, is not as common as primary open-angle glaucoma. This form of glaucoma can be either chronic (forming slowly over a long period of time) or acute (appearing suddenly). Its acute form is particularly serious and may cause vision loss within a day. Immediate medical attention is required to prevent vision loss. This form of glaucoma occurs when the drainage angle within the eye (formed at the junction of the cornea and the iris) narrows or becomes blocked. As we age, the lens within the eye pushes the iris forward, narrowing the drainage space. If fluid is no longer able to drain properly, it will build up, increasing the eye’s intraocular pressure and putting pressure on the optic nerve.
Glaucoma Symptoms
Primary open-angle glaucoma exhibits no early warning signs, develops gradually, and is completely painless. Damage to the peripheral vision occurs first, so most people don’t experience any symptoms until the visual field loss is significant and irreversible.
Acute angle-closure glaucoma typically presents suddenly with signs of nausea, red eyes, eye pain, blurry vision, and halos around bright lights. Those with chronic angle-closure glaucoma may not experience these symptoms.
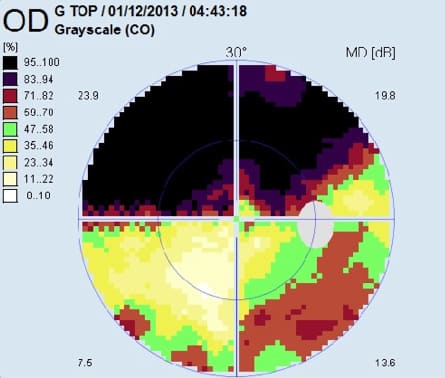
The asymptomatic nature of early stage glaucoma means that a comprehensive eye exam is often the only way to detect glaucoma before permanent vision loss occurs. During your eye exam, your optometrist will use both non-contact tonometry (the “air puff” test) and Goldman applanation tonometry. If you are suspected of having glaucoma, other tests will include retinal imaging, optical coherence tomography (OCT), visual field testing, and pachymetry.
Who is at Risk of Developing Glaucoma?
There are a variety of factors that can increase your risk of developing glaucoma:
- Age: Individuals over the age of sixty are more likely to develop glaucoma, and this risk factor increases slightly with each passing year.
- Select medical conditions: Conditions such as diabetes, high blood pressure, and heart disease may increase your risk of acquiring glaucoma and cause the disease to progress more quickly.
- Family history: Having a family history of glaucoma can increase your risk of developing the disease.
- Corticosteroid use: Patients that use corticosteroids for prolonged periods of time may be more likely to develop secondary glaucoma.
Your ocular anatomy, chiefly your corneal thickness and optic nerve appearance, may increase your risk of glaucoma. Other conditions such as retinal detachment and eye inflammation may also increase your chances of having glaucoma.
How is Glaucoma Treated?
Topical medication or surgery can slow or stop the progression of glaucoma. However, any vision loss that has already occurred is irreversible.
Topical Medications
There are several topical medications used to reduce intraocular pressure currently available on the market. Depending on the cause of your glaucoma, and how far it has progressed, your optometrist may prescribe one or more eye drops.
Surgery
There are several surgical procedures that may be used to reduce intraocular pressure, either as first line therapy or if topical medication is not sufficient.
Laser trabeculoplasty involves using a laser to increase fluid drainage through the trabecular meshwork (which is located at the junction between your cornea and iris) . However, the results may be temporary, and the procedure may need to be repeated.
Trabeculectomy involves creating a small drainage bleb within the eye, allowing excess fluid to drain into the vascular system.
Drainage valves or filtration implants are minimally invasive glaucoma surgery (MIGS) devices designed for patients with uncontrolled glaucoma. These procedures involve inserting a small device into the eye to help the aqueous fluid drain more efficiently.
For more information about glaucoma, please speak to your optometrist during your next appointment.